Needle Biopsy
A needle, or core, biopsy uses a needle alone or in combination with vacuum assistance to remove small pieces of tissue from potentially abnormal areas in your breast. The tissue is processed so that paper-thin slices are placed on a glass slide, stained and evaluated under the microscope.
No special preparation is needed in advance of these procedures and there are no limitations following them. You will be able to drive home and you may eat and take your medications as usual. Antibiotic coverage is not indicated in women with mitral valve prolapse.
These are safe procedures, but possible complications include:
- Infection
- Bleeding
- Pneumothorax (collapse of a lung) - an exceedingly rare complication, particularly when imaging guidance is used to sample the lesion
About the Procedure
Needle biopsies can be done using:
- Ultrasound guidance
- Stereotactic guidance
- MRI guidance
At the completion of any of these biopsy procedures, firm pressure is held over the area sampled for approximately 10 minutes, after which steri-strips are used at the site of the skin nick. You will be given the radiologist's business card, which includes their pager number, should you have any questions or concerns.
Ultrasound-guided needle biopsies
If an abnormality is seen with ultrasound, our preference is to do needle biopsies using ultrasound guidance; the patient is more comfortably positioned, no compression is needed and no radiation is used.
For the biopsy you are asked to lie on your back or be slightly turned to one side with your arm placed comfortably under your head.
The skin is cleaned with betadine and alcohol and then numbed with topical anesthesia (1 percent lidocaine). A small skin nick is made with a scalpel so that the tissue can be taken out of your breast, but it is so small that it does not require stitches. Using ultrasound guidance, the radiologist will advance the needle into your numbed breast until it reaches the lump. As the sample is taken you will hear a click in the room, after which the needle and sample are withdrawn from your breast and the tissue is placed in a formalin solution and sent to pathology for analysis.
This may be repeated several times, as needed, to adequately sample the area of concern.
Stereotactically guided needle biopsies
Stereotactically guided needle biopsies are used for lesions, such as calcifications, that may be seen only on a mammogram, not on ultrasound. Depending on the location of the lesion, you may be sitting or lying down. Your breast is compressed as is done for a mammogram and images are taken of your breast so that, in combination with a computer, a needle can be directed accurately toward the abnormality to be sampled.
The skin is cleaned with betadine and alcohol and then numbed with topical anesthesia (1 percent lidocaine) and a small skin nick is made with a scalpel so that the tissue can be taken out of your breast, but it is so small that it does not require stitches. The needle and sample are pulled out of your breast and the tissue is placed in a formalin solution and sent to pathology for analysis.
This may be repeated several times, as needed, to adequately sample the area of concern.
MRI-guided needle biopsies
MRI-guided needle biopsies are used for those lesions that are seen only with MRI.
An IV is started by a nurse so contrast can be given and you are asked to lie on your stomach. Your breast will be cleaned off with betadine and alcohol and then gentle compression is applied. Images are done first, then contrast is given and more images are done.
You will be taken out of the magnet so that your skin can be numbed with a local anesthetic (1 percent lidocaine). A needle is placed in your breast, after which your breast is scanned again to verify correct positioning of the needle with respect to the lesion to be sampled. If the needle is in the right place, samples are taken. Immediately after the biopsy is done, a small clip is deposited at the site of the biopsy and a mammogram is done to verify positioning of the clip; this clip serves to mark the site of the abnormality so it can be subsequently localized on the mammogram.
Your Results
Pathology results are generally available the next business day. An appointment is made for you to return to Breast Imaging so that the breast imaging radiologist can check the biopsy site and discuss biopsy results and recommendations with you.
It is important for the radiologist doing the procedure to correlate the imaging findings with what the pathologist describes on the samples. If the results are congruent (they "match" the imaging findings) and benign (non-cancerous), it may be that nothing more needs to be done. If atypia or premalignant changes are described, a referral to a surgeon is made to arrange for surgery to completely remove the area of concern. If cancer is diagnosed, an MRI — if not already done — and consultation with a surgeon are scheduled.
Rarely, if the imaging and pathology findings are not congruent (don't match), a repeat biopsy or consultation with a surgeon may be recommended.
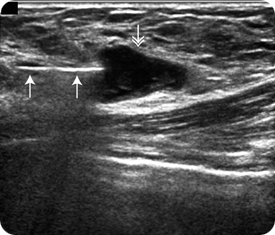 After the skin and breast tissue are numbed, a small nick — the size of a small paper cut — is made in the skin. Using ultrasound guidance, a needle (single arrows) is directed to the mass (double arrow) being sampled. When the needle is lined up with the edge of the mass, the sample is taken. Although ultrasound guidance is used in this example, the needle can also be directed to an abnormality by using stereotactic or MRI guidance.
After the skin and breast tissue are numbed, a small nick — the size of a small paper cut — is made in the skin. Using ultrasound guidance, a needle (single arrows) is directed to the mass (double arrow) being sampled. When the needle is lined up with the edge of the mass, the sample is taken. Although ultrasound guidance is used in this example, the needle can also be directed to an abnormality by using stereotactic or MRI guidance.
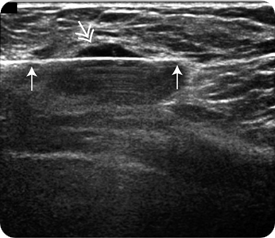 With needle and mass lined up, the needle is advanced through the mass rapidly to capture the sample. In this image, the needle (single arrows) is now seen through the mass (double arrow) being sampled. This process can be repeated as many times as needed to make sure that the area of concern is sampled adequately.
With needle and mass lined up, the needle is advanced through the mass rapidly to capture the sample. In this image, the needle (single arrows) is now seen through the mass (double arrow) being sampled. This process can be repeated as many times as needed to make sure that the area of concern is sampled adequately.
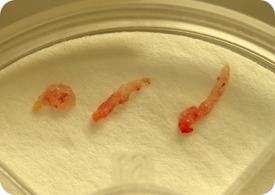 In this patient, three cores of tissue were obtained through different areas of the mass. The samples are sent to pathology for processing and evaluation.
In this patient, three cores of tissue were obtained through different areas of the mass. The samples are sent to pathology for processing and evaluation.
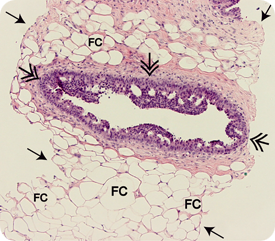 This image depicts a microscopic view of a core sample; arrows denote edge of core. After the tissue samples are processed they are sliced thinly, placed on a glass slide and stained so that they can be evaluated under the microscope. In this patient a duct (double arrows) is present with cells showing atypical ductal hyperplasia, a premalignant feature. The clear spaces are fat cells (FC), and stroma (pink material) is seen surrounding the abnormal duct and some of the fat cells.
This image depicts a microscopic view of a core sample; arrows denote edge of core. After the tissue samples are processed they are sliced thinly, placed on a glass slide and stained so that they can be evaluated under the microscope. In this patient a duct (double arrows) is present with cells showing atypical ductal hyperplasia, a premalignant feature. The clear spaces are fat cells (FC), and stroma (pink material) is seen surrounding the abnormal duct and some of the fat cells.
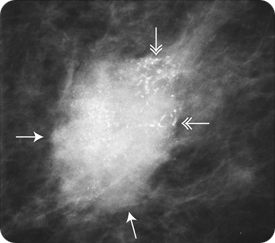 If core samples are done through an area of calcifications or, as in this patient, a mass (arrows) with calcifications (double arrows), an X-ray of the cores can be done to confirm that there are calcifications in the core samples.
If core samples are done through an area of calcifications or, as in this patient, a mass (arrows) with calcifications (double arrows), an X-ray of the cores can be done to confirm that there are calcifications in the core samples.
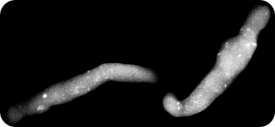 X-ray of two core samples confirming that calcifications (white spots) have been removed from the mass shown.
X-ray of two core samples confirming that calcifications (white spots) have been removed from the mass shown.
“All staff was extremely professional. On time with appointment, on time with exam — no waiting. Outstanding.”
- Excerpt from a VCU Breast Imaging patient satisfaction survey.


