National Grief Awareness Day: Compassionate care for others begins with ourselves
VCU Health team members found that developing strategies for coping with their own grief from the pandemic helped them be more effective providers for the patients and families they serve.
August 30, 2022
By Malorie Burkett, VCU College of Health Professions
National Grief Awareness Day takes place every year on Aug. 30. It's a day dedicated to the different ways individuals cope with loss while offering resources and support to those who are grieving. Whether someone is struggling with the loss of a loved one or undergoing significant life changes, Grief Awareness Day has shown that grief affects every person in its own distinct manner.
But what happens when grief affects those who dedicate their lives to providing support and care for others? A group of VCU Health team members has learned to face their own experiences with grief in hopes of becoming stronger, more effective providers for the patients and families they serve.
An insurmountable wave
Shortly after Sandra Menendez, B.S.N., graduated from her nursing program, she completed orientation as a VCU Health staff nurse, and set off to care for patients on the Medical Intermediate and Intensive Care Unit (MIICU). A couple of weeks later, the coronavirus pandemic forced Menendez and her colleagues to quickly learn what it meant to become COVID-19 nurses.
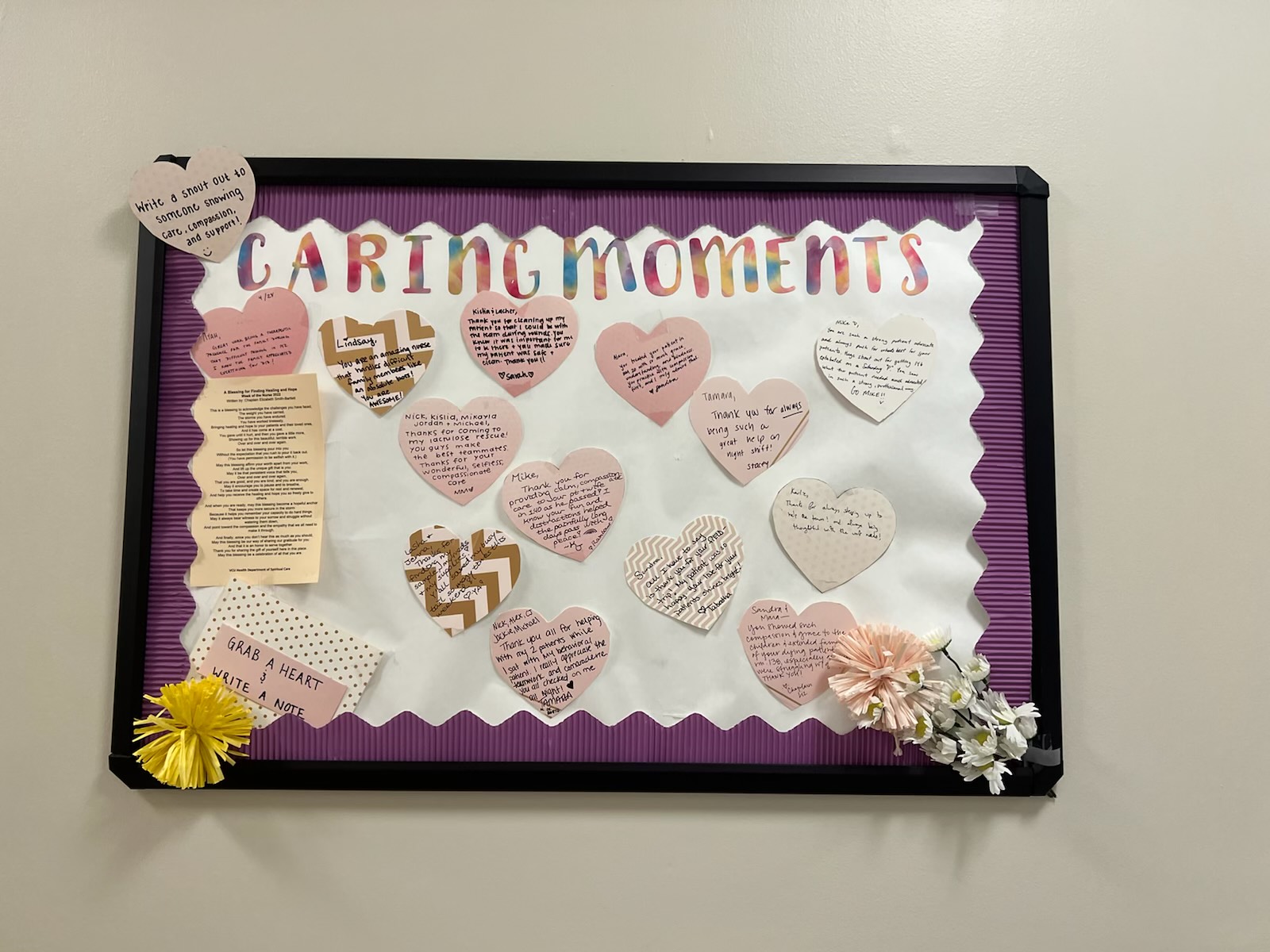 A board with paper hearts
A board with paper hearts
“It was lonely as a nurse because you're facing something that still had no good treatment and the only prevention at that time was your personal protective equipment,” Menendez said. “It was about asking your patient to trust you to provide care when nobody had answers yet.”
Menendez was experiencing her own difficulties while watching the rest of Richmond go through similar uncertainties. “It often felt just insurmountable, similar to being in the ocean and the waves are really big. The only way to get under the wave is to dive through it,” Menendez said. “Being a COVID nurse was like feeling the loneliness and helplessness with your patient.”
She recalled crying for patients when they died because she had gotten to know them personally and provided a hand to hold at the end. As the pandemic intensified, medical providers nationwide hit a compassion crisis. Like many providers across the country, Menendez's unit experienced burnout at unprecedented levels.
In August 2020, Elizabeth Smith-Bartlett was in her first year of the Virginia Commonwealth University College of Health Profession's Clinical Pastoral Education program. She recalled the different levels of grief throughout the MIICU unit.
“You could walk through those double doors and just feel it in your body, or at least I could. I think other people could too,” Smith-Bartlett said. “As a chaplain, trying to triage how I spent my time was really difficult because I think the reality was that everybody needed spiritual care on some level. Everybody needed support.”
Recentering compassion in caregiving
Both Menendez and Smith-Bartlett knew that something needed to be done. They, along with other colleagues, began to develop strategies to reincorporate compassionate care into nursing. For instance, the group organized “Cards, Cookies and Conversations,” an informal gathering inspired by the Pediatric ICU, where staff members wrote cards to family members of patients who passed away.
“I especially love this, because when nurses are talking about their patients who have passed on and writing cards to their family members, they're essentially sharing their secondary traumas,” Menendez said. “When we sit and listen to them share stories about their patients and what that end-of-life process was like for them, we're creating a safe place.”
The group also started a comfort care closet, which holds blankets, men's shaving supplies and an assortment of hair products as well as essential oils. Additionally, they added supplies to create fingerprints of patients, which they provide to loved ones at end-of-life care. In an ICU, the number of line streams and tubes can make it challenging to feel safe enough to touch a patient, Menendez said, but a family member can sit and hold the fingerprints so they feel like they're touching their loved one.
A bulletin board also allows coworkers to recognize one another for moments of compassionate care and share meaningful notes of encouragement. Menendez said these and other initiatives have been helpful in allowing the nursing team to process trauma and provide better care for patients.
After organizing these initiatives for patients, family members and themselves over the past couple of years, Menendez partnered with Smith-Bartlett and others to form their own unit committee, known as the Bereavement and Compassionate Care Committee. Officially established earlier this year, Menendez and staff nurses Azia Mills, Jordan Jones and Gia Balducci organize events that are open to all nurses, doctors, support staff and anyone who wishes to take part.
“If I've learned anything over the past two years, it's that I have to make sure that I'm filling my own cup because I can't pour from an empty cup,” Smith-Bartlett said. “There are times where we really have to scrape the bottom, but that should be the exception and not the rule, and that's been my growing edge over these past two years. I want to be able to do this work because I feel deeply called to it, but I also need to do it in a way that isn't just taking everything out of me.”
Smith-Bartlett said she was deeply moved that MIICU leadership and staff were the drivers in recentering compassion in their caregiving. “Watching some of those nurses at the bedside is just inspirational. I think they provide as much spiritual care as we do,” she added.
The 'give and take' of grief
Today, the committee continues to plan activities and events for patients and each other. Menendez also remains in touch with some of the family members she met at the onset of the pandemic, including the family of a patient who stayed in the unit for over 100 days. After leaving VCU Health, the patient was transported to an out-of-state hospital, but he passed away shortly afterward.
“I was there on his sickest days. I helped him stand for the first time. His care team and I took him on field trips throughout the hospital. His wife and I took him outside for the first time in a hundred days … wrapped in seven blankets in 20-degree weather,” Menendez said. “We would spend hours after my shift talking about anything and everything. He was the best part of those years; he got me and many of my coworkers through the pandemic. It's very sad not to have him here anymore. He and his family were a true gift to our unit.”
Menendez said she misses him every day, but that patient is the reason she continues to do what she does.
“I think that all human relationships are like a two-way street. You give and take,” Menendez said. “I think that's especially important in grief. You give to your patients and their family members, but you can also take these beautiful, terrible moments.”
Menendez believes that she has grown as a person and a nurse through grief.
“We have new graduate nurses and I just want so much for them to not be afraid of grief, bereavement and sadness, because it is a give and take,” she said. “It is the most human thing you can do.”
You can join the College of Health Professions in honoring Grief Awareness Day this year by lighting an electronic or wick candle from wherever you are at 7 p.m., or whenever is most convenient. You can also simply turn on your cellphone light. For more information, contact Stephanie Hamilton at slhamilt@vcu.edu.




