September is national suicide prevention month
Perspectives on suicide from a psychiatrist and a patient
September 26, 2022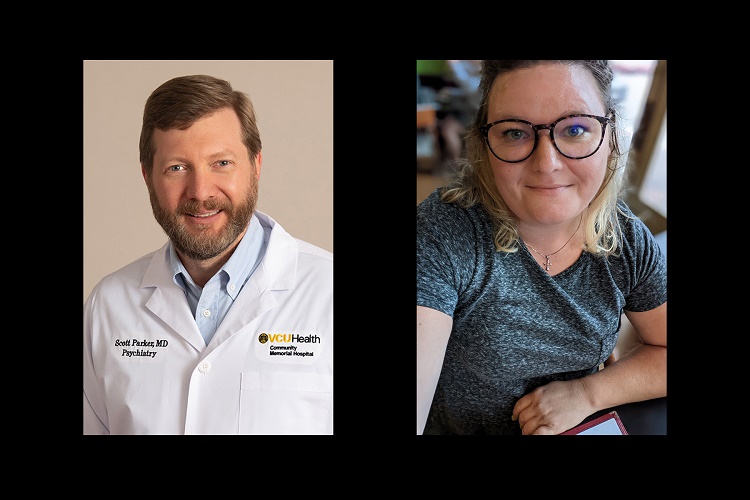
The United States has about 46,000 deaths by suicide each year, compared to 700,000 worldwide. To raise awareness of these devastating statistics, VCU Health Community Memorial Hospital wants to help educate the public, give tips on how to help someone and amplify the resources available in our community. We spoke with Scott Parker, M.D., a psychiatrist at CMH Behavioral Health in South Hill. One of his patients was willing to share her story, as well.
Who is at risk?
"The single-most determining factor of suicide is previous attempts," Parker said.
He's seen an increase in demand for his services, but he attributes it to psychiatrists retiring at a faster rate than new ones starting to practice.
Certain demographics can determine a higher rate of suicide, such as race, residence, occupation and sexual orientation. For example, Native Americans and whites are more likely to commit suicide than other races.
People in rural areas are more at risk than their urban counterparts. Working in a rural area, Parker sees how people have more access to guns and less access to care. There are plenty of therapists in our area, but insurance is a limiting factor for many.
"People in the construction industry are more likely to experience substance abuse," Parker said. "Nursing has come to the forefront during the pandemic as a high-stress job."
The LGBTQ+ community is more susceptible to feeling ostracized.
"As society becomes more accepting of sexuality, that will improve," Parker said. "It's a long-standing problem that transgender individuals have a higher rate of being targeted, verbally abused and physically assaulted, which leads to increased rates of depression, anxiety and suicidal thoughts."
A patient's perspective.
Lori Kidd, of Brodnax, is a four-time suicide attempt survivor.
"People need to know more about suicide," she said. "It's real. It's not a joke. People are going through tough times and need comfort, not judgment. Sometimes they just need a hug."
She's lived in the area all her life and understands the struggles in a rural community.
"There's no outlet; no social interaction," Kidd said. "We don't have bowling alleys, movie theaters or other ways to get together. Drug activity is rampant."
Kidd has benefited from calling the suicide lifeline.
"They once texted me for three hours," she said. "It was very helpful; they talk to you like a person with emotions."
She has a good support network of friends who reach out and tell her not to go through with it. They remind her of her family that depends on her and would miss her if she was gone.
"COVID isolation has made everything worse," Kidd said. "The economy is not helping, either. It has put pressure on people in rural areas."
But things are looking up for Kidd. She's starting a new job in retail management and launching her side photography business. She's got a family that relies on her, and she is making new relationships.
What can we do to help?
The 9-8-8 Suicide and Crisis Lifeline's slogan for National Suicide Prevention Month is "Be the one to…" followed by five simple steps: Ask, be there, keep them safe, help them stay connected, and follow up.
Ask. The last thing anyone wants to do is ask someone if they're thinking of killing themselves. It's awkward and uncomfortable.
"Asking does not increase the risk," Parker said. "It's harder for the person asking than the person who feels suicidal. The best approach is to be direct."
The person needing help will feel relieved and being able to talk about it may even reduce the chances of them going through with it.
Be there. If someone is confiding in you, don't be judgmental. Use active listening by making eye contact and repeating their concerns to make sure they feel heard.
Keep them safe. Guns are the most lethal way of ending life.
"The most important thing you can do for someone having suicidal thoughts is to get guns out of the house," Parker said. "Removing the deadliest means of suicide is half the battle."
Help them stay connected. People need to have a network of resources and support. Make sure they know where to turn in an emergency. The new lifeline is now easy to remember: 9-8-8.
Follow up. Check back in to make sure the person is improving, especially if they've recently been discharged from a hospital. Support groups, churches and therapy are all great options.
What resources are available in the community?
First and foremost, call 9-8-8 in an emergency.
There are many local counselors in the 434 area code. It may be difficult to find one that accepts your insurance. Visit vcu-cmh.org and click on Services: Behavioral Health to see a list of resources in the community.
Psychiatrists are meant to diagnose mental illness and manage medications, while psychologists, therapists and social workers can provide more in-depth therapy.
CMH Behavioral Health has telehealth options for college students and those who live out of the area, though on-site visits may be required. Call (434) 584-5400 to make an appointment with a psychiatrist.




