Novel approach to treating arrhythmias sets Pauley Heart Center apart
High-dose targeted radiation therapy provides 'great outcome' for patient with end-stage ventricular tachycardia.
July 06, 2022 Getty Images
Getty Images
Alexander Reeves, M.D., was 84 and semi-retired. The former chair of neurology at the Geisel School of Medicine at Dartmouth College had enjoyed being mentally and physically active for decades.
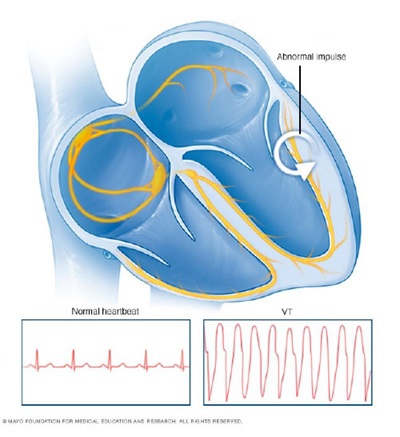
But ongoing ventricular tachycardia threatened his life. Ventricular tachycardia is most often due to heart muscle damage. Its resultant scarring causes an abnormally rapid heartbeat, which substantially increases risk of sudden death.
When conventional treatments failed and Reeves' condition was end stage, he turned to VCU Health. In April 2021, VCU Health Pauley Heart Center physicians, in collaboration with colleagues from the Department of Radiation Oncology and Radiology, used a high-dose of targeted radiation to successfully destroy those parts of Reeves' heart they believed to be causing his arrhythmias.
Reeves became the first VCU Health patient to undergo radiation therapy for ablation of refractory VT — a new technique still rarely performed nationally.
Since treatment, Reeves has had no full or even partial ventricular tachycardia events, and his high doses of antiarrhythmic medications are being tapered and discontinued.
“We had a great outcome. He's an impressive success,” said Kenneth Ellenbogen, M.D, director of clinical cardiac electrophysiology and pacing at VCU Medical Center.
Radiation treatment advantages
 A major advantage of the procedure is that it is outpatient, fast and doesn't require general anesthesia.
A major advantage of the procedure is that it is outpatient, fast and doesn't require general anesthesia.
“The patient lies on the table for less than 15 minutes, and we can stop their VT,” Ellenbogen said, though planning prior to the ablation is extensive.
Patients with ongoing ventricular tachycardia typically undergo ablation by catheter, which directs heat energy or extreme cold to the areas of the heart causing the misfire and scars the tissue to prevent further issues. The catheter ablation procedure is invasive, takes several hours, requires general anesthesia and carries a 50% chance that one treatment will not stop arrhythmias from recurring. None of this happens with radiation therapy.
Ellenbogen estimated “a couple hundred patients at most worldwide” have received the radiation treatment, which was pioneered by the Washington University School of Medicine in St. Louis. Data on the long-term effects of treating VT with radiation is limited, he said, adding that the therapy poses its own risks to the heart. The procedure is a last measure for severely ill patients for whom catheter ablation procedures have been ineffective.
Reeves' physicians initially attempted catheter ablation but had been unable to completely reach the part of his heart causing the misfire — one of the consequences of prior open-heart surgery in 2013 to repair a valve. Reeves also suffered from major side effects caused by drugs doctors had hoped would help manage his arrhythmia.
Pauley offers one last option
“When I was asked if I wanted to do this new procedure, I said fine, we've got nowhere else to go,” Reeves said. “I was on this terrible poison, amiodarone. It's last resort stuff — any physician will tell you that — with awful complications.”
A defibrillator implanted in Reeve's heart to shock it back into rhythm during VT felt “like being shot, but there was no wound,” he said.
Ellenbogen and Santosh Padala, M.D., another VCU Health electrophysiologist who, before his death in 2021, had an interest in ventricular tachycardia ablation. They planned their strategy for radiation therapy along with their colleagues Greg Hundley, M.D., director of the VCU Health Pauley Heart Center and clinical director of noninvasive cardiology at VCU Medical Center; Cory Trankle, M.D., assistant professor in the Division of Cardiology in the School of Medicine and a Pauley Heart Center noninvasive cardiologist; John D. Grizzard, M.D., an associate professor of radiology in the School of Medicine and noninvasive cardiovascular imaging section director for VCU Medical Center; and Elisabeth Weiss, M.D., a clinical professor in the School of Medicine and a VCU Medical Center radiation oncologist. Padala performed Reeves' prior catheter ablation and was able to determine that part of the circuit was under scar tissue from prior open-heart surgery.
The team mapped the problem area near Reeves' mitral valve via electrocardiogram and imaging technologies, then applied stereotactic body radiation therapy, a noninvasive radiation procedure most commonly used to treat cancer.
At one year post-surgery, Reeves is doing well. He's still recovering from the mental and physical impacts of treatments prior to radiation therapy, but he as an exuberant outlook.
“I may have a new lease,” he said. “I figure I've used up seven of my nine lives. I probably have two left.”




