Debunking 5 common myths about ALS – What you need to know
Because ALS is a rare disease, figuring out what is and isn’t true can be tough. The head of the VCU Health ALS Clinic helps us find answers.
July 24, 2025 Approximately 5,000 people in the United States are diagnosed with ALS each year, according to the Centers for Disease Control and Prevention. (Enterprise Marketing and Communications)
Approximately 5,000 people in the United States are diagnosed with ALS each year, according to the Centers for Disease Control and Prevention. (Enterprise Marketing and Communications)
By Haley Tenore
Trying to find reliable information when you or your loved one has a medical condition with an unknown cause and no definitive cure can be a serious challenge. From limited depictions of patients on television to being bombarded with myths online, it’s easy to fall into traps of misinformation.
For a rare disease like ALS (amyotrophic lateral sclerosis) that only affects 4 to 6 people out of 100,000, it could even be harder to find someone credible to talk about these concerns.
Kelly Gwathmey, M.D., understands what that’s like. As the director of the VCU Health ALS Clinic, she regularly speaks with patients and their caregivers about some of the common misconceptions about ALS.
Gwathmey spoke with VCU Health News to debunk some of the myths surrounding this rare disease.
MYTH 1: ALS progression looks the same for everyone.
WHAT ARE THE FACTS?
Like many health conditions, ALS looks different for every person who has it. The way the disease first presents itself, its progression and life expectancy after symptoms begin to develop can differ significantly.
“About 30 to 40% of patients will have bulbar onset disease, which affects their speech and swallowing muscles first, whereas the remainder have limb onset, which can start in a hand, arm, or leg,” Gwathmey said. “Someone who develops slurring of their speech and difficulty swallowing looks quite different than someone who has a foot drop and is in a wheelchair.”
At the VCU Health ALS Clinic, Gwathmey says about 10% of patients will live more than 10 years, however, the average life expectancy after symptoms begin is between 2 to 5 years.
MYTH 2: There is nothing that can be done to treat ALS.
WHAT ARE THE FACTS?
While there isn’t a cure for ALS, that doesn’t mean there aren’t any options to treat the disease. There are therapies and medications available that can help patients.
“In terms of the treatment approach with this disease, it's a combination of multidisciplinary care that improves clinical outcomes, including life expectancy and quality of life. Additionally, we have three disease-modifying therapies – Riluzole, Tofersen, and Edaravone – that slow the progression,” Gwathmey said.
The sooner these medications are given to a patient, Gwathmey says, the better they work. That’s why patients should seek medical attention as soon as they recognize the signs of ALS. Some of the first signs of ALS can include muscle twitching, muscle weakness and difficulty swallowing or speaking.
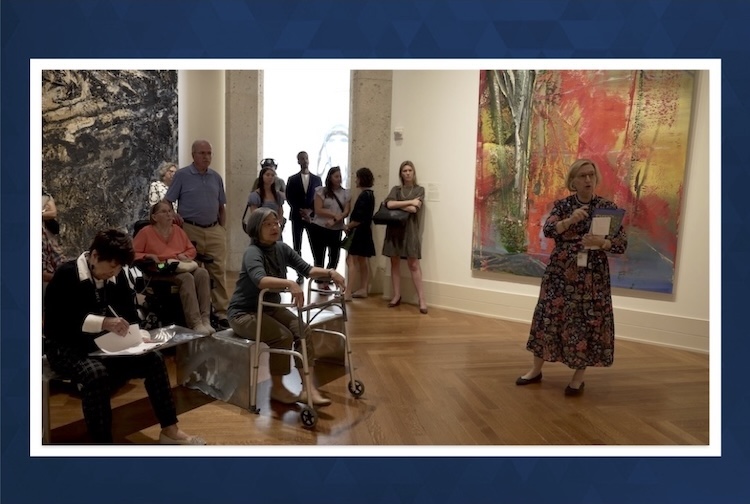
Additionally, VCU Health’s multidisciplinary approach to care includes a wide range of providers with expertise in treating and managing ALS, including a social worker, occupational therapist, respiratory therapist, registered dietician and nursing staff who support the patient and caregiver with any changes that come with the disease.

VCU Health's ALS clinic and research program is the largest of its kind in Virginia. (Enterprise Marketing and Communications)
MYTH 3: ALS is painless.
WHAT ARE THE FACTS?
As ALS progresses, it can cause muscle loss, loss of nerve function and eventually paralysis. Because of this, there is sometimes a misconception that patients don’t feel pain. But this doesn’t tell the whole story, as patients can experience stiffness or cramping, which can be very painful.
Additionally, “because patients have neck weakness, they're struggling to keep their head upright all day. That results in some strain on their neck, muscles and discomfort that way,” Gwathmey said.
MYTH 4: ALS only impacts the muscular and nervous systems.
WHAT ARE THE FACTS?
Because ALS is a motor neuron disease, it can be easy to assume that it only impacts a person’s ability to move. While most people who have ALS are primarily impacted this way, some can also experience cognitive decline and dementia.
Some patients can also experience an onset or worsening of anxiety or depression due to the changes that come with ALS. Patients can also experience the pseudobulbar affect, which causes unexplained, uncontrolled fits of laughing or crying.
MYTH 5: We know what causes ALS.
WHAT ARE THE FACTS?
Myths have come and gone about potential causes of ALS. Though 10% of people with ALS have a family history and approximately 15% may have a genetic cause of the disease, most don’t.
There was also a myth that Lyme disease could potentially be a cause, but experts agree that there likely isn’t a link between the two conditions. Some have also suggested that certain lines of work might cause ALS, though there still isn’t a definitive answer.
“What causes sporadic disease? It's like getting struck by lightning,” Gwathmey said. “It’s thought to be a combination of environmental exposure and genetic predisposition. Environmental exposure can be through occupational hazards, playing contact sports or military service. We know a lot of different risk factors that seemingly lower the threshold to developing ALS, but we don’t have a perfect formula of what needs to happen to develop ALS.”