After lifesaving heart procedure, Virginia man witnesses son’s NFL dreams come true
VCU Health gave Trent Henderson more time for life, love and nine growing sons – including an NFL running back.
December 02, 2025 Trent Henderson (right) with his son, TreVeyon, and wife, Jennifer, at the 2024 College Football National Championship. (Contributed photo)
Trent Henderson (right) with his son, TreVeyon, and wife, Jennifer, at the 2024 College Football National Championship. (Contributed photo)
By Jeff Kelley
In April, Trent Henderson and his family — namely, his son TreVeyon — were anxiously sitting on a couch when the phone rang.
On the line: The New England Patriots.
The crowd that had gathered at their party — family, friends, supporters — erupted in cheers and tears. The Hopewell, Virginia, native and standout Ohio State University running back had been picked up in the second round of the 2025 NFL Draft.
“It just didn’t seem real. To see this little kid’s dream come true, and to have that moment with him and to be alive and share it with him, it was amazing.” Trent said. “We are so proud of him.”
For Trent, “to be alive” and to share that moment with TreVeyon – and more with his eight other sons – is made possible by a life-saving heart-pumping device implanted at VCU Health.
Family at the heart of a life-altering choice
Trent had been diagnosed with congestive heart failure in his mid-20s, which meant regular doctor appointments over the years. During a routine cardiac catheterization at a local community hospital to assess his heart, doctors found the 47-year-old to be in end-stage heart failure.
Trent was immediately transferred to VCU Medical Center, where heart specialists connected to VCU Health’s Hume-Lee Transplant Center and Pauley Heart Center gave him three to six months to live. They also gave him options: A heart transplant and, while he waited for transplant, a left ventricular assist device (LVAD) to keep his heart properly functioning.
With advances in technology, [LVADs] work well and people are living with them just as long as they are with a transplant.
Tyna Justice, RN, BSN, LVAD coordinator at VCU Health
A few weeks later in December 2013, a surgical team implanted the LVAD device into his heart.
But for Trent, the LVAD isn’t about what it does, but what it gives him. His “whole reason for living” is to be the father to nine boys.
“The LVAD has helped me live and travel and watch my kids grow up over the last 12 years without any issues,” he explained. “I wanted to see them grow up. I wanted to be there for their graduations, their games, their big moments.”
An LVAD on him, a team behind him
The LVAD (or simply VAD) is used either as a bridge to transplant or as destination therapy for patients who are not transplant candidates. While he would qualify for a transplant, Trent decided against it and instead chose to live with the device.
“I’ve got my reasons,” he said. “Right now, the LVAD’s doing its job. I’m still here. I’m still a dad.”
While life‑sustaining, an LVAD involves major lifestyle adjustments, such as managing batteries and protecting the external equipment, as well as being vigilant about device maintenance and infection prevention. In recent years, housing LVAD equipment has become far more discreet and adaptable — often kept in a sleek vest or crossbody bag, like in Trent’s case — allowing patients to move through daily life with comfort and confidence, often without others even noticing.
At the same time, changes made by the United Network for Organ Sharing (UNOS) in 2018 to the heart transplant requirements mean LVAD patients often wait longer for transplantation, since being stable with a device places them lower on the priority list.
“That means every patient pathway is going to be different, and it’s not going to be an option for every patient,” said Kathryn Abernathy, MS, RN, ACCNS-AG, CHFN, VCU Health’s manager of transplant services. “LVAD patients who are awaiting transplant typically do very well and rehabilitate and eventually get back to their lives.”
The lifestyle changes and support system needed to stay healthy
Whether the choice is made for a heart transplant or an LVAD, lifestyle modifications are required for the rest of a person’s life.
“A lot of people think that once you get a heart transplant that you just go and live your life. But it’s not that — there’s a lot of maintenance, follow-up and medication,” said Tyna Justice, RN, BSN, one of VCU Health’s three VAD coordinators. “With advances in technology, VADs work well and people are living with them just as long as they are with a transplant.”
Justice has cared for Trent over her last six years at VCU Health and says he is the kind of patient a clinical care team dreams of having.
“He’s independent, he takes his medications, he comes to his appointments and he knows when to call us if something’s wrong. That makes all the difference,” she said. “We’ve seen him through tough times and celebrated his successes. It’s about trust and knowing him as a person, not just a patient.”
The LVAD has helped me live and travel and watch my kids grow up over the last 12 years without any issues.
Trent Henderson, VCU Health patient
For patients living with an LVAD, having a strong support system is as essential as medical care.
Clinical social workers meet with patients before surgery, evaluating whether they have the help and stability at home needed to succeed after leaving the hospital. Over time, those relationships grow into lasting bonds.
“I’ve known Trent since before the LVAD went in,” said VCU Health clinical social worker Megan Maltby, LCSW. “You’re with them for life. We celebrate the highs, like graduations or new grandchildren, and we grieve the lows alongside the family.”
Social workers guide families through both the emotional toll and the practical realities of living with an LVAD.
“It’s a special bond that’s very unique,” Maltby said. “And it’s very important, because there’s a level of trust that’s built.”
With the LVAD, there’s more time for milestones
The time given to Trent has mattered the most — and given him the particularly unique experience of watching one of his nine boys rise from Hopewell High School football standout to college star to New England Patriots draft pick.
From following his recruitment by powerhouse programs to proudly watching him shine as an Ohio State Buckeye, Trent has been there for son TreVeyon’s journey. “And without this LVAD, I wouldn’t have been here to see it,” he said.
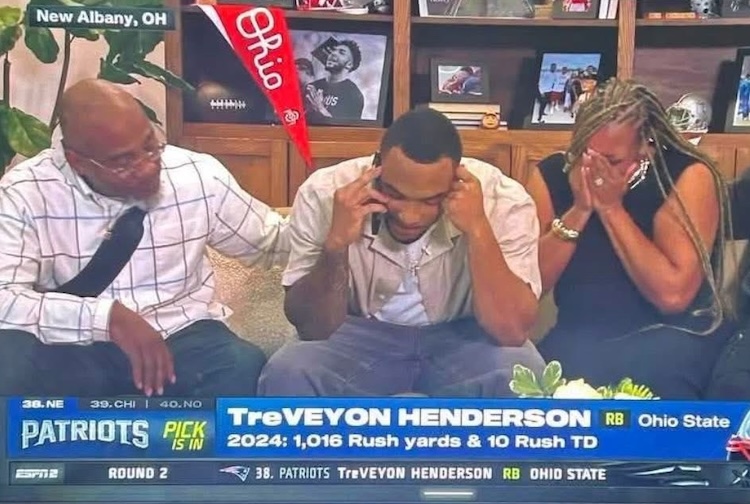
Trent Henderson credits the LVAD for helping him be healthy enough for his children’s big milestones, including when his son, TreVeyon, found out that he was drafted to play for the New England Patriots. Left to right: Trent Henderson with TreVeyon Henderson and Lakeesha Hayes, TreVeyon’s mother. (Contributed photo)
That excitement spread to the clinical care team.
“When we saw his son get drafted, it felt like it was our son, too. That’s how invested we are in these families. I’m an Alabama fan, but we became Ohio State fans because of TreVeyon,” said Maltby, whose NFL team is the Washington Commanders. “Now I have to be a Patriots fan — but only for the Hendersons.
Having an LVAD has given Trent a chance to keep experiencing milestones with his family.
“It’s like having a second heartbeat you can hear,” he said. “It’s always there, reminding me that I’ve got another chance.”
That chance is sustained not just by the device, but by the team behind him — doctors, nurses, coordinators and social workers — all working together to help him live his best life.
For Trent, that bond has meant everything. “This LVAD gave me time,” he said. “More time with my boys. That’s all I want.”
What to know about left ventricular assist devices (LVADs)
Inspired by Trent’s story? Read more about our patients and providers




