What to know about left ventricular assist devices (LVADs)
VCU Health’s collaborative care team provides a lifesaving option for a growing number of patients with advanced heart failure.
December 11, 2023 Patients can live for many years after receiving an LVAD procedure. Patients Dammien Mason and Trent Henderson both received LVADs in recent years, with Henderson hitting his 10 year LVAD anniversary in December 2023. (Medtronic / VCU Health Hume-Lee Transplant Center)
Patients can live for many years after receiving an LVAD procedure. Patients Dammien Mason and Trent Henderson both received LVADs in recent years, with Henderson hitting his 10 year LVAD anniversary in December 2023. (Medtronic / VCU Health Hume-Lee Transplant Center)
By Caroline Ward and Sara McCloskey
Providing a seamless continuum of care for heart patients is at the core of an important collaboration between VCU Health Hume-Lee Transplant Center and Pauley Heart Center.
Since 2006, cardiovascular surgeons have implanted more than 500 durable mechanical devices aimed at improving blood circulation. Of those procedures, more than 400 left ventricular assist devices (LVADs) and over 120 total artificial hearts have been implanted.
Recently, VCU Health completed their 100th HeartMate3™ LVAD procedure, which is the most advanced device of its kind. It has significantly modernized the field of LVAD therapy, setting the standard with innovation and outstanding clinical outcomes for patients.
“Our successful outcomes represent the many patients who have been given a second chance at life through these advanced treatment methods,” said Keyur Shah, M.D., chief of advanced heart failure at VCU Health Pauley Heart Center. “It is a strength and benefit to patients to have the involvement of both Hume-Lee and Pauley care teams. The collaboration of both centers ensures excellent resources and expertise to take care of LVAD patients even after the patient leaves the hospital.”
Shah, who researches heart failure and mechanical assist devices, shares more details about LVADS as well as the resources for heart patients who are interested in pursuing this procedure.
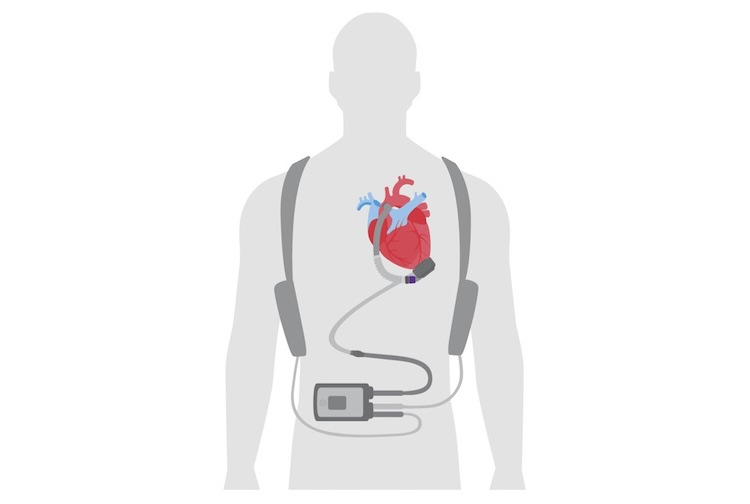
Illustration of a left ventricular assist device (LVAD). (Photo contributed by Abbott)
What is a left ventricular assist device?
A left ventricular assist device, also known as an LVAD, is a mechanical pump that is surgically implanted into the patient's chest to assist the left ventricle of the heart in pumping blood. It is used to support the heart's pumping function when the heart is too weak to do so on its own.When is an LVAD used?
LVADs are primarily used in patients with severe heart failure, a condition where the heart is unable to pump blood effectively to meet the body's needs. Symptoms for these patients may include severe shortness of breath, swelling, frequent hospitalizations, fatigue and failing of their organs.LVADs are often considered when other treatments, such as medication or lifestyle changes, have not been successful, and the patient is awaiting a heart transplant (as a bridge to transplant) or as definitive therapy for those who are not transplant candidates.
How does an LVAD work?
An LVAD is connected to a patient’s left ventricle and aorta. It draws blood from the left ventricle and pumps it into the aorta, which then distributes oxygen-rich blood throughout the body. The device is powered by an external controller and batteries or an implanted power source, which continuously monitors and controls the LVAD's operation.Is the LVAD a permanent solution?
LVADs can be a long-term solution for patients who are not candidates for heart transplantation. For others, it serves as a bridge to transplant, supporting the patient while they await a suitable donor heart. In some cases, the LVAD may also be removed if the patient's heart function improves with time or treatment.What are the risks and complications associated with LVAD implantation?
While LVADs can significantly improve the quality of life for patients with severe heart failure, there are potential risks and complications. These can include infection, bleeding, clotting, device malfunction and stroke. Patients with an LVAD require close medical monitoring and care to manage these risks.What is the recovery process like for LVAD recipients?
Recovery varies from patient to patient. Initially, patients may stay in the hospital for several weeks to monitor the device and manage any post-surgery complications. Over time, patients can resume most normal activities.Patients are followed closely post-procedure to adjust medications and the LVAD device if needed. There are dedicated LVAD locations at VCU Health Stony Point 9000 and VCU Medical Center, where they are frequently seen by providers and monitored.
There are also support groups to help patients during their journey, to answer questions and provide additional education. The LVAD coordinators are heavily involved and frequently speak to LVAD patients and caregivers further providing support and guidance.
Can LVAD patients live a normal life with this device?
Many LVAD patients experience a significant improvement in their quality of life. They can engage in regular activities, travel, and spend time with family and friends. However, adherence to a strict medication and care regimen, regular medical follow-ups and lifestyle adjustments are essential for a successful long-term outcome.How can someone become a candidate for an LVAD?
To be considered for an LVAD, patients typically go through a comprehensive evaluation by a cardiac care team to assess their overall health, heart function and the severity of their heart failure. The decision to implant an LVAD is made on a case-by-case basis, considering the patient's medical history and specific needs.