VCU Health researchers find neurological clues for treating overactive bladders
By uncovering connections between the bladder and the brain, the research team aims to help people regain control and confidence in their lives.
November 29, 2023 Carrie Hillman, who is being treated for urinary issues at VCU Health, listens as Linda Burkett, M.D., describes the inner workings of the pelvic floor at a recent visit to the GreenGate clinic. (VCU Enterprise Marketing and Communications)
Carrie Hillman, who is being treated for urinary issues at VCU Health, listens as Linda Burkett, M.D., describes the inner workings of the pelvic floor at a recent visit to the GreenGate clinic. (VCU Enterprise Marketing and Communications)
By Olivia Trani
Carrie Hillman hasn’t let much get in the way of living life to the fullest. When she and her husband married, she juggled raising children, attending college and taking odd jobs to make extra money for her family.
“It took me 15 years to earn my degrees in psychology and counseling. When our boys were little, I also typed papers, sewed dresses, and all sorts of other things because we were as poor as church mice,” she laughed.
Hillman worked as a school counselor for several years, later becoming the director of a private school in San Antonio. Since retiring and relocating to Richmond, Hillman has dedicated her time to her church community, working as a musician and parish administrator. She also volunteers for Bible Study Fellowship International, helps with fundraisers for local charities, spends time with her grandchildren and participates in her neighborhood’s book club.
“If you could see my office, I have piles of documents for different projects. You could say I’m 79 years young. My body tells me that I’m 79, but I don’t feel it in my mind,” she said.
Despite her various activities and responsibilities in daily life, Hillman is always aware of one thing: where the nearest bathroom is.
In her 30s, Hillman had a hysterectomy to remove growths in her uterus, which ended up creating significant challenges for her bladder.
“Sometimes I would need to go to the restroom 10 to 15 times during the day,” she said. “I always wore black in case I ever had an accident, and I was very conscious of how close I was to a bathroom at all times, especially when we traveled.”
Hillman is one of the participants involved in a VCU Health study to better understand the connection between the bladder and the brain in hopes identifying some of the neurological factors directly causing people to develop overactive bladders. The preliminary data, presented in October at the American Urogynecologic Society’s annual scientific meeting, is providing new insights into what regions of the brain are linked to abnormal bladder function.
“This research is a significant step in finding a way to more efficiently care for our patients,” said Linda S. Burkett, M.D., a urogynecologist at VCU Health who is leading the project. Urogynecologists specialize in treating women with pelvic floor issues. “The long-term goal is to create a test that can provide predictive information about what types of treatments may be most effective for restoring normal bladder activity.”
Losing bladder control
People with overactive bladders experience a frequent or urgent need to urinate. The condition can cause individuals to feel a sudden impulse to use the bathroom several times during the day and night, and potentially lead to accidental leakage.
“Usually, when you feel the need to urinate, you give your body the signal when the time is appropriate and all your reflexes work together. However, when you lose that control, the bladder muscle contracts without your body’s permission and you risk experiencing leakage,” said Burkett, who is an assistant professor in the Virginia Commonwealth University School of Medicine’s Department of Obstetrics & Gynecology.
Having an overactive bladder can affect a person’s quality of life in several ways. This includes losing sleep from needing to use the bathroom multiple times overnight, and reluctance to travel long distances out of fear of having an accident in public.
Various factors can increase the risk of developing an overactive bladder, including neurological disease, nerve damage, obesity and aging. According to the Urology Care Foundation, as many as 30% of men and 40% of women in the United States have symptoms of overactive bladders.
There are several therapies that can help patients manage their symptoms, from weight loss and physical therapy to medications and surgeries, however the biological mechanisms that cause this condition are not well understood.
“We don’t have a great understanding of exactly where the defect has truly occurred,” Burkett said.
Carrie Hillman is one of several women participating in a VCU Health study led by Linda Burkett, M.D. to better understand the neurological factors causing people to develop overactive bladders. (Left to right: Carrie Hillman and Linda Burkett) (VCU Enterprise Marketing and Communications)
Finding the connection between the brain and bladder
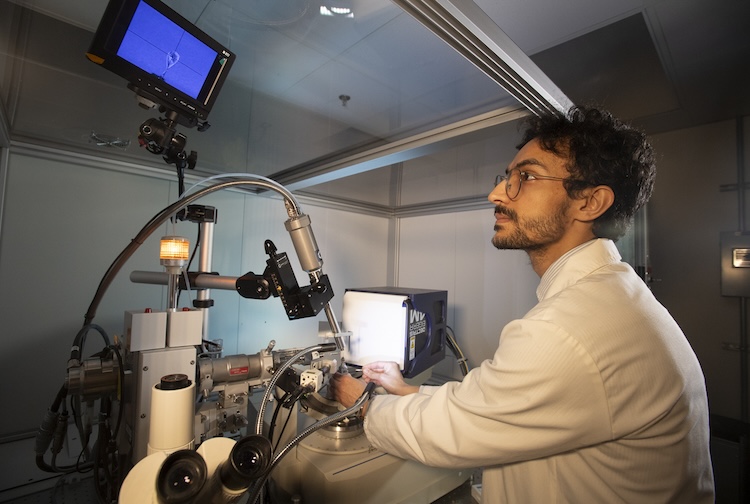
For this study, conducted in a research space at the VCU Health Adult Outpatient Pavilion, Burkett and her colleagues monitored the brain activity of female participants with and without overactive bladders.
Each participant wore a sensor device the size of a matchbox to measure changes in their bladder’s blood oxygen levels, a metric that can be used to estimate the fullness of a person’s bladder as they drink fluids. At the same time, participants wore head caps equipped with sensors that can measure blood oxygen levels in the outermost regions of the brain. For the brain to function properly, our blood vessels supply oxygen to our brain cells, and when certain regions of our brain are in use, more blood flows to those areas. Using these sensors — an approach called functional near-infrared spectroscopy — researchers can determine which regions of the brain are active and inactive as a person’s bladder fills.
The initial results revealed that, as bladders became full, participants with overactive bladders had significantly lower blood oxygen levels in the brain's prefrontal cortex compared to participants with normal bladders. The prefrontal cortex is the region of the brain involved in decision-making, problem-solving and self-control. The findings suggest that the prefrontal cortex helps people voluntarily control their full bladders until they find a bathroom, whereas people with less activity in this part of the brain may have less voluntary control of their bladders.
Burkett is continuing to collect data for this study, and with additional research, she hopes to be able to detect unique patterns in the brains of people with overactive bladders. She also plans to conduct similar experiments to see if patients have better control of their bladders after receiving treatment.
“We are now starting to look into how a person’s brain patterns change after receiving treatments for overactive bladder. We want to know whether the brain goes back to normal or if the body uses a different neural pathway to solve the issue,” Burkett said.
Burkett is one of four VCU scholars who are funded by the National Institutes of Health’s Building Interdisciplinary Research Careers in Women’s Health grant. The funding provides junior faculty with enough funds to kick-start their research until they secure a larger independent grant.
“This grant is very interdisciplinary and mentor-driven. For this project, I work with colleagues in the Department of Surgery and the Department of Mechanical Engineering, who bring a unique set of skills and expertise to the table,” Burkett said. “By coming together, we’re helping bridge the gap in women’s health research.”
Taking charge of your health
After decades of managing her symptoms with medication and alternative treatments, Hillman recently sought long-term treatment options at VCU Health.
“My mother also had trouble with controlling her bladder, and she was afraid to go out because of the problems she was having. When I realized I was letting my bladder issues dictate my life in a similar way, I decided that I didn’t have anything to lose and a lot to gain by seeking medical help,” she said.
Hillman also credits her close friend, Mimi Bennett, who encouraged her to prioritize her health.
“Mimi had worked as a nurse practitioner at VCU Health for years, and she convinced me to finally take the bull by the horns,” Hillman said. “She is my biggest fan and encourager.”
After consulting with Burkett, Hillman underwent surgery to receive a neurostimulator designed to treat overactive bladders. The implanted device sends a small current, like a pacemaker, to improve communication between the bladder and brain.
"If what I'm doing helps others down the line and contributes to their future well-being, then that's a win-win situation and answer to prayer,” she said.