
VCU Health leads clinical trial for new treatment to help people with bowel control problems
The three-year study is a collaboration between clinical experts at VCU Health and researchers at Cellf Bio to provide more options for treating a health issue that impacts 1 in 3 adults in their lifetime.
February 28, 2024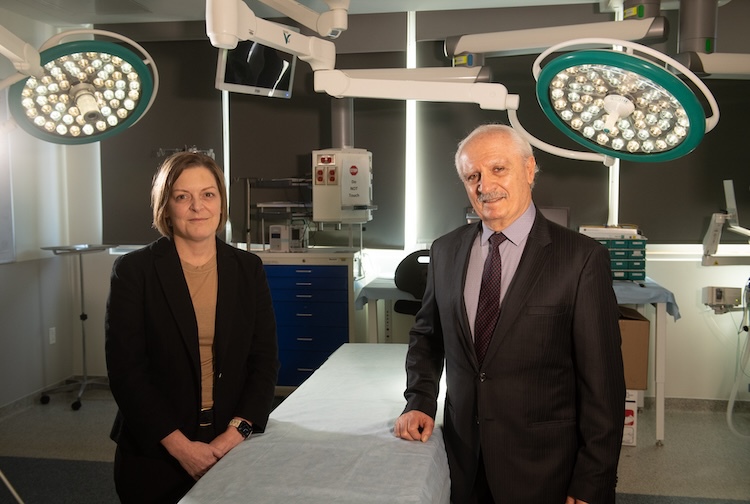 Jaime Bohl, M.D., and Khalil Bitar, Ph.D., pictured in the Christine B. and David E. Cottrell Surgical Innovation Suite at the VCU School of Medicine. (VCU Enterprise Marketing and Communications)
Jaime Bohl, M.D., and Khalil Bitar, Ph.D., pictured in the Christine B. and David E. Cottrell Surgical Innovation Suite at the VCU School of Medicine. (VCU Enterprise Marketing and Communications)
By Olivia Trani
A research team at VCU Health is leading a clinical trial to assess a novel treatment for fecal incontinence or sudden loss of control over bowel movements. The therapy involves implanting a bioengineered sphincter derived from the patient’s native cells to help them regain control of their bowels.
The implantation surgery for the clinical trial is being led by Jaime Bohl, M.D., an associate professor in the Department of Surgery and chief of the Division of Colon and Rectal Surgery at Virginia Commonwealth University’s School of Medicine.
“There hasn't been a new treatment for this condition in well over ten years, and we have seen a lot of excitement from patients over the possibility of a new therapy,” she said. “We’re getting phone calls from patients all over the country who are asking about their eligibility for the clinical trial.”
Bohl and her team successfully completed the first implantation last summer and will be enrolling eligible patients over the next three years.
"We are very pleased with the progress of the clinical trial thus far," said Khalil N. Bitar, Ph.D., founder and CEO of Cellf Bio, a Richmond-based biotech company that designed the bioengineered sphincters. "This is a major step forward in the development of BioSphincter as a potential treatment for fecal incontinence."
Fecal incontinence: A common yet covert health issue
Fecal incontinence is the involuntary loss of stool or fecal material. According to estimates from the National Institutes of Health, 1 in 3 adults will experience fecal incontinence during their lifetime, and people are more likely to develop the condition as they age.
“A lot of patients are embarrassed about this condition and will stop going to social outings for fear of not being able to find a toilet and having an accident,” Bohl said. “Many of them won't even talk to their physicians or families about the condition. They start to narrow the framework of their day, social structures and friendships. It can be really isolating for people.”
Fecal incontinence has many causes and one is internal anal sphincter dysfunction. The internal anal sphincter is a ring of smooth muscle located inside the rectum. When this muscle becomes weakened or damaged – such as from a chronic illness or injury – a person can lose control of their bowel movements.
There hasn't been a new treatment for this condition in well over ten years, and we have seen a lot of excitement from patients over the possibility of a new therapy.
Jaime Bohl, M.D., chief of the Division of Colon and Rectal Surgery at VCU School of Medicine
A number of therapies and procedures can help people maintain better control of their bowel movements, including medications, physical therapy, surgery and nerve stimulation. However, some people can still experience symptoms even after seeking treatment.
“We see that there are some patients who have tried all the treatments available and still have persistent bowel control problems, which is incredibly frustrating for them,” Bohl said.
From bench to bedside
The BioSphincter is made from stem cell tissue that Bohl and her surgical team collect from the patient’s sphincter and small intestines through a biopsy. The biomedical team led by Bitar at CellfBio then uses the tissue sample to grow the implant over six to eight weeks. The patient subsequently undergoes surgery to receive the bioengineered implant.
“Many therapies are designed to manage symptoms of fecal incontinence rather than restore function. That’s where our technology comes in,” Bitar said. “The bioengineered tissue is intended to improve or replace the internal anal sphincter muscle, which helps us control our bowels. The BioSphincter is also the first implant of its kind to be made of the patient’s native tissue.”
Bitar began his work on this technology as a research professor and director of pediatric gastrointestinal research at the University of Michigan before relocating to Wake Forest University to be a professor and director of gastrointestinal programs. It was there that he connected with Bohl, who was working as an assistant professor and colorectal surgeon at the time. Since meeting, they have worked together for more than 12 years to further develop the BioSphincter implant.
Through this collaboration, the researchers have been working hand in hand to take this innovation from the bench to the bedside. An expert surgeon and clinical researcher, Bohl has led preclinical studies on the therapy and helped navigate the approval process for the clinical trial.
“Partnerships in science and medicine are critical, as it’s incredibly hard for one person to do it all,” Bohl said.
Treating patients with bowel control problems in Richmond and beyond
The clinical trial will be enrolling patients who have tried all available therapies for fecal incontinence yet still experience symptoms.
While the main goal of the clinical trial is to assess the safety of the implant, the researchers will also measure the technology’s effectiveness as a treatment for fecal incontinence. The researchers will evaluate the physical function of the bioengineered muscle tissue, the frequency and severity of fecal incontinence experienced by the patient, as well as whether a patient’s quality of life changes following the implant.
The study will be enrolling patients initially at VCU Health and then at additional sites.
“We decided to hold the clinical trial at multiple sites to show this procedure could be done anywhere in the country,” Bohl said. “We wanted to show that the BioSphincter can be made in the lab here and shipped to wherever the patient is, as well as show that this surgery can be performed by other colon and rectal surgeons.”



