Patient testimonial: How a rare aortic aneurysm repair saved Latarsia
The 43-year-old is optimistic about the coming decades after a lifesaving surgery at Pauley Heart Center

At the root of her fear was an extensive history of female first- and second-degree maternal relatives dying from complications related to brain and aortic aneurysms. At the age of 9, Greene’s childhood was shaped by the loss her mother, age 36, due to a ruptured aneurysm.
“The year I turned 36, I didn’t do much of anything because I was convinced I was going to die,” she said.
When her sister died from a brain aneurysm at 43, the same age Greene received her surgery, “all that did was exacerbate my fears,” she said.
Greene’s nightmare caught up with her six years ago when she felt a “searing, burning pain” in her back near the kidneys. She was later seen at a Fredericksburg, Virginia, emergency room and was immediately transferred by helicopter to VCU Medical Center to receive specialized care, where physicians confirmed she suffered a tear, or dissection, in the inner layer of her aorta.
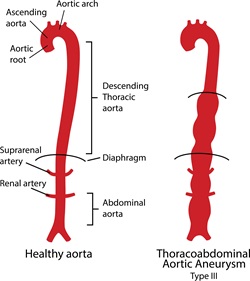
Dissections put aneurysms at greater risk of rupture, said VCU Health vascular surgeon Daniel Newton, M.D.
“The wall of the aorta has multiple layers, and if it acutely stretches, there can be a partial tear,” Newton said. “Blood flow is supposed to be contained within the inner layer. When it tears, you get blood flow in between the layers, and that weakens the vessel.”
After close monitoring of the aneurysm for months, on March 30 Greene was operated on by Newton and VCU Health cardiothoracic surgeon Katherine Klein, M.D., with assistance from a VCU Health cardiac anesthesiologist, and specialists in neuromonitoring and blood profusion. For eight hours, the team undertook the maximally invasive repair of the aortic aneurysm, which had a diameter roughly the size of a peach and spanned the length of Greene’s abdomen into her chest.
Newton added that full open repairs are increasingly rare because stents, which can often be inserted through tiny incisions, are a minimally invasive solution. But because VCU Health geneticists say Greene’s family history indicates she may have inherited a disorder that causes weak arterial tissue, stents were not an option because the devices can tear weak tissue.
Open surgery better ensured a lasting aortic repair for Greene, but risked damage to her brain, spinal cord and vital organs. The operating team preventatively monitored blood profusion and electrical activity in the brain and spinal cord, and maintained blood pressure and blood flow to all vital organs. If changes had occurred, the team would have notified Newton and Klein, so they could change their approach, said Sam Ingram, a certified neuro-physio interoperative monitor on Greene’s surgical team. Ingram monitored Greene’s brain function.
“Surgery is a really big day. My job is to help protect everything after that day,” Ingram said. “Are you a piano player? Do you have grandchildren to pick up? No one wants to come back from surgery not being themselves.”
The surgeons sewed a graft to the small portion of healthy aorta that remained in Greene’s chest above the aneurysm, reinforced the device with
felt and connected each branch to vital organs to the new graft. In all, eight reconnections were made to arteries from her chest down to the iliac arteries, located in the front of Greene’s hips. In patients with normal aortic tissue, groups of vessels can sometimes be attached to the graft simultaneously, but Greene’s weak tissue required surgeons to painstakingly attach the vessels one by one, Newton said. VCU Health Pauley Heart Center is one of the only facilities in Virginia with the expertise and equipment necessary for an open thoracoabdominal aortic aneurysm repair.
“She’s not the only one of our patients going back to work after this type of surgery,” Newton said. “I think that is from our technical choices and strong collaboration between vascular, cardiac, the intensive care unit and anesthesia that have given us some really good outcomes.”
Greene had a remarkably fast recovery from surgery. “It saved my life,” she said. “I feel that as long as I keep up with my after care and checkups and keep my blood pressure under control, I will be fine.”

Join our Pauley Consortium composed of patients, friends and advocates.