Early Pioneers Inspire Today’s Cath Lab
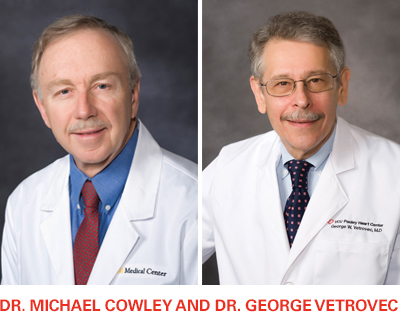
In its early years, the VCU cardiac catheterization lab was dedicated to diagnosis. That all changed when Dr. Michael Cowley and the lab’s new director, Dr. George Vetrovec, introduced balloon angioplasty to Virginia in 1979.
“It was the first time people with coronary disease could be treated without surgery. That’s obviously a huge thing to be able to offer to patients,” said Dr. Zachary Gertz, director of the Cardiac Catheterization Lab.
Over the years, as catheters, imaging and techniques have improved, cardiologists have been able to treat more patients, with increasingly complex interventions. In 2018, Pauley’s cardiologists performed 3,882 procedures in the hospital’s four cath labs, which operate around the clock.
Pauley draws many high-risk patients that other institutions turn away, such as frail patients that require temporary heart pumps during their interventions. “We still get the most challenging cases from all over the state,” said Gertz.
Gertz was recruited to the faculty in 2012 to develop the structural heart disease program, following his involvement in the first study for transcatheter aortic valve replacements [TAVRs]. In 2017, Dr. Barbara Lawson joined the team, and like Gertz, performs procedures such TAVRs and percutaneous closure of atrial septal defects and patent foramen ovale.
He has watched the evolution of TAVRs. At first, only patients at high risk of complications during surgery could undergo the procedure, then medium-risk patients were approved. Now, research indicates its suitability for low-risk patients.
He also took part in early studies for MitraClips, which are implanted in patients with leaky mitral valves, and sees mitral valve replacements and tricuspid valve repairs on the horizon.
Dr. Jose Exaire performs the lab’s most challenging interventions, on vessels with chronic total occlusion [CTO]—meaning they are completely blocked. He has an 85-90% success rate of successful PCIs for these patients. In only 10% of the attempts is he unable to penetrate the arterial wall, using a variety of approaches.
“There are always new developments to try to aid this complex procedure and thanks to that, we can attempt to tackle more complex patients,” said Exaire.
Not all the cases involve the heart; Exaire and Dr. Deepak Thomas also perform procedures on blockages in other parts of the body.
“These include, but are not limited to, interventions for lower extremity peripheral artery disease, upper extremity disease such as subclavian stenoses and renal artery interventions,” said Thomas. “Most cardiologists recognize that coronary disease rarely occurs in isolation and a full understanding of the `vascular’ part of cardiovascular can only help our patients in their overall wellbeing as we attack arterial injury from a medical, interventional and preventative standpoint.”
Research in the lab is ongoing, including one study in which stem cells are injected into heart tissue to regenerate areas that have experienced cell death after a heart attack.
Innovation has long been a part of the lab, said Gertz. “George [Vetrovec] started a cath lab that has the reputation of doing the best and most complicated things in Richmond and throughout the state,” he said, “and I just want to maintain that, along with our same high qualities and outcomes.”
Congratulations to Dr. Gertz on being named director of the Cardiac Catheterization Laboratories this May! Stay tuned for more news about his appointment in our next issue.
Back to Autumn-2019

