Urinary incontinence is common, but it’s not normal
VCU Health Community Memorial Hospital urologist explains treatment options.
December 29, 2023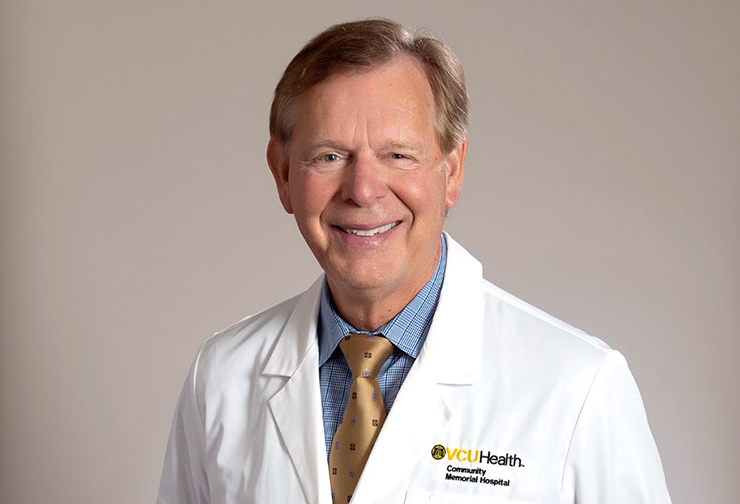
According to the American Urological Association, a third of people ages 40 and older in the United States suffer from urinary incontinence, which is the loss of bladder control.
“A lot of people believe incontinence is just part of getting older, but that's not true,” said John Pearson, M.D., a board-certified urologist with VCU Health Community Memorial Hospital (CMH). “Urinary incontinence is common, but it's not normal. So, if you're having incontinence problems, you don't have to live with them. People that have urinary incontinence have a higher incidence of hip fractures and several other non-urologic problems. It's worthwhile to see your primary doctor to get a referral to a urologist.”
We’re sharing common questions patients have about urinary incontinence, which Pearson addressed as part of a recent talk for CMH’s Community Outreach Education (C.O.R.E.) program.
Why are people hesitant about getting help?
A lot of people are embarrassed about it. They don't want to go out in public and be on the lookout for a bathroom all the time. Some patients tell me that they’re afraid they don’t smell good, and that keeps them home. It's important to deal with this health problem and try to make it better.What are symptoms and causes of an overactive bladder?
If you're going to the bathroom more often than you used to, if you must go to the bathroom in a hurry and you can't get there in time, if you get up at night more than one time to go to the bathroom, those are all symptoms of an overactive bladder.Causes can range from a relaxed pelvic floor to decreased signals from the brain to the bladder. Types of drinks and foods and when they are consumed also cause incontinence.
What causes urinary incontinence?
Urinary retention is just the opposite of incontinence. Retention means you can't get all the urine out when you go, or any of it out. This occurs more often in men than women. When the bladder gets to a certain overfilled state, it just starts leaking out. You don't really urinate. You just leak.Stress incontinence occurs when you accidentally urinate while lifting something, coughing, sneezing, laughing, or even getting up out of a chair. It is usually caused by pelvic floor relaxation. The pelvic floor gets stretched out in women who've had children, women who are overweight and just from age. The bladder sits on the floor of the pelvis, and when the pelvis gets stretched out and the bladder sags, it pulls the urethra open, and it can't close tight enough to give you control anymore.
Urge incontinence happens when the nerve telling the bladder to hold it isn't working anymore. Medications can relax the bladder, allow it to fill without increasing pressure, or give you the sensation that you need to go. And then when you get the urge to go, you can get to the bathroom in time and are able to go like you're supposed to.
How is urinary incontinence treated?
The first step is to diagnose it and determine what sort of incontinence it is and what's causing it. A lot of people can improve with just lifestyle changes. Being selective on what you drink or eat, and changing when you stop drinking liquids before you go to bed are both good things to try.There are oral medications that have varying side effects and can be very expensive. If none of the oral medications work, or nothing works you can afford, or you have side effects from them, then we can go on to advanced therapies.
We always try to use methods to get the symptoms under control that are short of surgery or interventions. We always want to do the least invasive thing to get you better.
What are some lifestyle changes that can improve bladder control?
Caffeine is one of the worst culprits of urinary incontinence. Coffee, tea and soda will all increase your voiding symptoms. Spicy food affects some people. Constipation can also cause it.Symptoms of overactive bladder can frequently be controlled by what's called timed voiding; when you've determined how long your bladder will hold before it starts to go and then urinate before that happens. So, if you go more than two hours and you can't get to the bathroom in time, then make yourself go to the bathroom every 90 minutes and just go by the clock rather than waiting for your bladder to tell you to go when you're not going to be able to control it.
Kegel exercises are primarily for stress incontinence. They don't do much for urge incontinence. The muscles in your pelvic floor can get lax with age and with the bladder sagging and frequently exercising, those muscles can improve your stress incontinence. Basically, when you have a bowel movement and cut off the stool at the end, you tighten your pelvic floor. And if you tighten it, relax it, tighten it and relax it, that's what the Kegel exercises are. That will strengthen your pelvic floor. The only problem is you've got to do it forever for it to work.
What interventions do providers offer?
Percutaneous tibial nerve stimulation is when we put a little needle in the tibial nerve down in your ankle. It's like acupuncture. It stimulates a tibial nerve. It's a weekly treatment for six weeks, and it may improve frequency, urgency and incontinence for months. And it can be redone. It's minimally invasive. The needle is tiny. It's a temporary procedure, but it does work very well for some people.Sacral neuromodulation is when we implant a device the size of a silver dollar in the fat of your buttocks. We put a wire down to that nerve and stimulate it. And it wakes that nerve up and tells your bladder to relax and gives your control back. It's very effective. Everything is internal and the battery lasts about seven years. We can do a trial run in the office to test it before doing the surgery.
Sign Up for VCU Health Community Memorial Hospital’s E-Newsletter